The Learning Health System and Decision Support
I was first introduced to the learning health system in 2014, when I had the privilege of attending an IHI Patient Safety Conference in Florida. Brent James, now Chief Quality Officer at Intermountain Healthcare, explained the learning health system as a five-step process (1):
- Identify a high priority clinical process where there is evidence for a need to improve practice.
- Build an evidence-based best practice guideline around that process.
- Integrate the guideline into clinical workflow as decision support within a clinical system that has the capability to track what happen.
- Use the data to create a learning loop. This involves feeding back the data to clinicians so that they can review and reflect on the results of applying the evidence-based guideline.
- Modify the guideline and associated protocols to reflect the learning from the data.
This process has been a cornerstone of my vision for the Decision Support Programme over the years. What makes it so powerful is the way it blends;
- classic evidence-based practice
- data-driven quality improvement
- and practitioner ownership of the learning from the evidence.
It points to the need to work across the traditional silos of literature-based evidence and evidence derived from practice or service data, so that we can blend the best of both worlds to inform the best possible decisions about health and care.
Brent James’ outline brings to life in a practical way the definition provided by the Institute of Medicine in 2007: “ a system in which “science, informatics, incentives, and culture are aligned for continuous improvement and innovation, with best practices seamlessly embedded in the delivery process, [with] patients and families active participants in all elements, and new knowledge captured as an integral by-product of the delivery experience.”(2)
Charles Friedman, a thought leader in this field, helpfully summarises the enablers of a learning health system (3):
- Every patient's characteristics and experiences are securely available as data to learn from.
- Best practice knowledge derived from these data is immediately available to support health-related decisions.
- Continuous improvement is enabled through ongoing review of this data.
- A socio-technical infrastructure enables this to happen routinely, with a significant level of automation, and economy of scale.
- Stakeholders within the system view these activities as an integral part of their culture.
For us in Scotland, the need to make this vision a reality is more pressing than ever just now, as we face the challenges of renewal and recovery from the COVID pandemic, rising costs and inequalities in access to care.
We have within reach many of the enablers Friedman highlights. Healthcare data and knowledge are growing exponentially, and we have increasingly powerful technology to release their untapped potential. For example, digitisation of health and social care record systems enables us to capture and store patient data at scale; analytics platforms for extracting meaning from large population datasets; wearables, sensors and monitoring systems to extract meaning from daily activity data, and decision support tools using structured rules from research knowledge or data-driven methods such as machine learning.
Through quality improvement and patient safety programmes, our understanding has grown of human factors, behavioural change, and the systems and processes needed to embed change and translate evidence into practice.
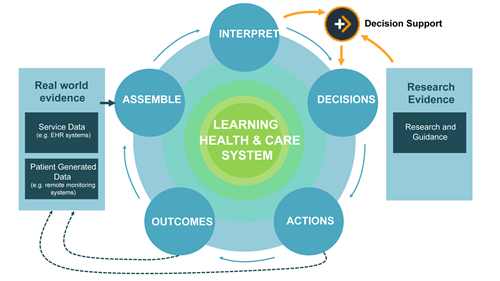
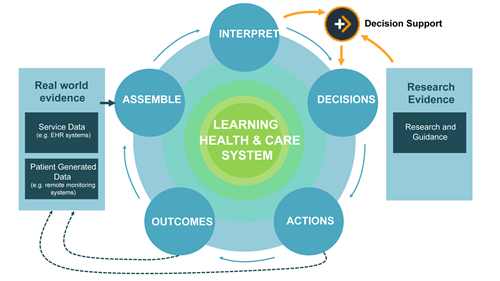
Decision support has a pivotal role to play in connecting these different elements of the learning health system. The diagram below illustrates how decision support can adapt rules based on research knowledge to reflect insights from real-world data that show the reality of practice and outcomes in our context. It can then facilitate change in practitioner and patient/citizen behaviour by making this blended evidence easy to access and use in decisions about health and care.
Learn more about the Decision Support Programme on our website.
- https://intermountainhealthcare.org/blogs/topics/transforming-healthcare/2016/06/4-steps-to-a-learning-healthcare-system/
- M. McGinnis, D. Aisner, and L. O. Olsen, “The Learning Healthcare System,” National Academies Press, Washington (DC), USA, 2007. [Online]. Available: https://www.nap.edu/catalog/11903/the-learning-healthcare-system-workshop-summary
- Friedman, CP, Allee, NJ, Delaney, BC, Flynn, AJ, Silverstein, JC, Sullivan, K, Young, KA. The science of Learning Health Systems: Foundations for a new journal. Learn Health Sys. 2017; 1:e10020. doi: 1002/lrh2.10020